Amoebic Dysentery also called as Amoebiasis, Protozoal Dysentery, Entamoebiasis or Amoebiasis Protozoal Infection. It is an infection of the intestine that may involve the colon, soft tissues, lungs or liver. Dysentery is an inflammatory disorder of the intestine, and more of the colon that results in severe diarrhea containing blood, mucus and pus in the stool. The frequency of stool passages is 10-30 times per day. This infection is caused by Entamoeba hystolytica. The disease can be acquired by ingestion of food or water or by sexual contact: orogenital, oroanal, proctogenital
Entamoeba hystolytica is a parasitic protozoan of humans which is under the classification of Sarcodina of the Protozoans. These species are in vitro at 37˚C. They are widely distributed in aquatic habitats and are packed with food vacuoles with host cells & bacteria. More protozoa are recognized by a motile feeding stage called the trophozoite that requires ample food and moisture to remain active. A large number of species are also capable of entering into a dormant, resting stage called a cyst when conditions in the environment become unfavorable for growth and feeding.
II. Morphological Description
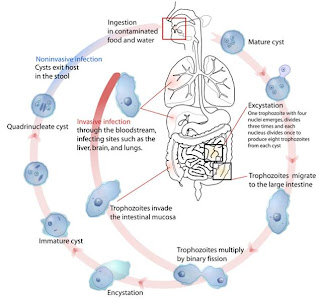
Entamoeba hystolytica has three stages in its life cycle:
1. The trophozoite
2. The precyst
3. The cyst
1. The trophozoite - 0.1-0.6mm in size
- contains RBC in its inclusion; feeding
stage
- invasive stage; has an irregular
finger-like shape(pseudopodium)
- move by extending a pseudopodium pulling
the rest of the body forward (called
the amoeboid movement)
- fixative: PVA (polyvinyl alcohol)
2. The precyst - immature; forms a wall during encystment -
the trophozoite cell rounds up into a sphere,
and its ectoplasm secretes a tough, thick
cuticle around the cell membrane.
- cyst wall is composed of chitin which
provides resistance to environmental factors
- has Chromatoidal bars - short, rod-shaped
structures w/ rounded ends
3. The cyst - mature; 0.1 - 0.2mm in size
- infective stage (upon excretion with the feces)
- cyst maturation involves 2 rounds of nuclear
replication w/o cell division and cysts with 1-4
nuclei are found in the feces
- Fixative: formalin
Pathogenecity of E. hystolytica:
A cyst secretes 4 trophozoites. There, the trophozoites attach by fine pseudopods , multiply, actively move about and feed. The severity of infection depends on the strain of the parasite, inoculum size, diet, and host resistance.
The secretion of lytic enzymes by the amoeba seems to induce apoptosis of host cells. This means that the host is contributing to the process by destroying its own tissues on cells from the protozoans. It invasiveness is also a clear contributor to its pathogenicity.
E. hystolytica actions:
1. Amoeba secretes enzyme
2. Dissolves tissues
3. Penetrate deeper mucosa
4. Causes erosive ulcerations (dysentery = bloody, mucus-
filled stools)
Parasite proteins:
- Eh-lectin - responsible for the lysis within minutes of adhering to them in the presence of extracellular calcium. It is involved in resistance to complement mediated lysis.
- Amebapore - to lyse ingested bacteria
- Proteases - enzymes that degrade other proteins
III. Signs & Symptoms
Clinical amoebiasis exist in intestinal and extraintestinal forms. The initial targets of intestinal amoebiasis are the cecum, appendix, colon, and rectum. The amoeba secretes enzymes that dissolve tissues and it actively penetrates deeper layers of the mucosa, leaving erosive ulcerations. This phase is marked by dysentery, abdominal pain, fever, diarrhea, and weight loss. The most life-threatening manifestations of intestinal infection are hemorrhage, perforation, appendicitis, and tumorlike growths called amoebomas. Lesions in the mucosa of the colon have a characteristic flask-like shape.
Extraintestinal infection occurs when amoebas invade the viscera of the peritoneal cavity. The most common site of invasion is the liver. Here, abscesses containing necrotic tissue and trophozoites develop and cause amoebic hepatitis. Another rarer complication is pulmonary amoebiasis. Other than infrequent targets of infection are the spleen, adrenals, kidney, skin, and brain.
IV. Diagnostic/Lab Tests
- Microscopic stool for examination - For cyst or trophozoites characteristics
- ELISA tests of stool - For E. histolytica antigens
- Sigmoidoscopy
- Serological testing - For presence of antibodies to the pathogen (+)
V. Period of Communicability
The microorganism is communicable for the entire duration of the illness.
VI. Incubation Period
> severe infections = 3 days.
> subacute and chronic forms = lasts for several months.
> average cases = 3 to 4 weeks.
> Extraintestinal amoebiasis/hepatic abscesses = years
Asymptomatic carrier excrete 15M cysts/day while chronic carriers excrete them seldom.
VII. Prognosis
With proper treatment, most individuals recover fully withing 2-4 weeks after beginning of treatment. Without treatment, however, mortality can be high and serious medical complication can develop such as liver, lung or brain infection (extraintestinal infections). Because medication cannot keep you from getting infected again, repeat episodes of amoebiasis may occur if you continue to travel or live in areas where amoebas are present.
VII. Epidemiology
E. hystolytica is harbored by chronic carrier whose intestines favor the encystment stage of the life cycle. Cyst formation cannot occur in active dysentery because the feces are so rapidly flushed from the body; but after recuperation, cysts are continuously shed in feces. The amoeba is thought to be carried by one-tenth of the world's population, and it kills up to 100,000 people a year. Occurrence is highest in tropical regions such as Africa, Asia and Latin America. Although the prevalence of the disease is lower in the United States, as many as 10 million people could harbor the agent.
VIII. Prevention
Purification of water by means of chlorination, however may not be enough, so boiling and introduction of iodine is require. Cyst forms can be destroyed by boiling water, dessication, direct sunlight, heat or by adding 200ppm of iodine. The best way of preventing the disease is by washing your hands.
IX. Treatment
No vaccine yet exists for the amoeba. Effective treatment usually involves the use of drugs such as iodoquinol, which acts in the feces, and metronidazole (DOC) or chloroquine, which works in the tissues. The principle behind for metronidazole is it binds to protozoal DNA to cause loss of helican structure and strand breakage, it also inhibits nucleic acid synthesis and causes cell death. The most common drug used is Flagyl. Dehydrometine is used to control symptoms but it will not cure the disease. Lost fluid and elecrolytes are replaced by oral or intravenous therapy this includes ORS, NSS and Dextrose.
No comments:
Post a Comment